The healthcare industry today has come a long way. It’s no longer the one-dimensional, transactional type of operation that people have experienced for decades.
It’s now one of the largest industries globally and interaction expectations have changed. Patients are not only looking for quality medical care – they also want a quality experience too, and are comparing it to what they receive from other businesses and brands.
By fostering a positive patient experience, a medical organisation can create better health outcomes and achieve higher patient retention rates, which is a win for everyone.
Let’s discuss how to make the patient journey a positive and memorable one, and why that matters.
Improving the patient experience through customer feedback
In order to take a more patient-centric approach, healthcare facilities are developing new strategies to optimise communication and engagement. One popular strategy is to proactively gather feedback.
By doing this, healthcare facilities can utilise customer feedback to map the patient journey and assess their experience to:
- identify underlying issues and opportunities.
- continually improve service standards.
- identify processes that aren’t working for staff and/or patients.
Feedback can also help you raise the service standard across the board.
For patients, capturing their feedback demonstrates that their input is appreciated, heard and valued. Internally, this feedback aids in establishing service KPIs and fostering a culture of innovation within your workforce.
So, when implementing a feedback cycle, you’re making a positive move towards holistic improvements to build better relationships with everyone involved.
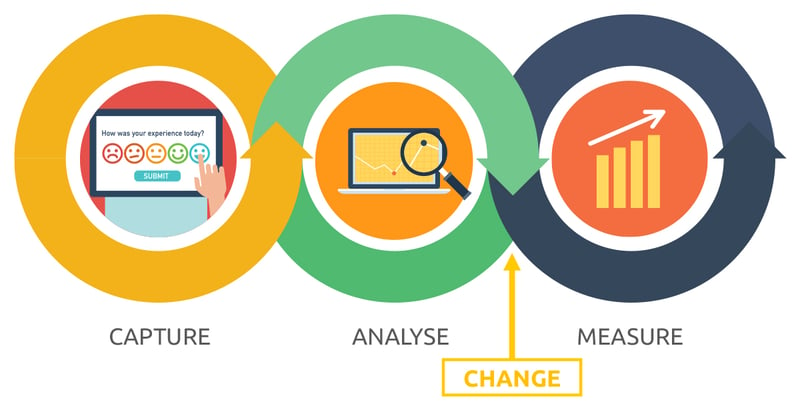
Just remember that applying the right techniques to collecting and interpreting feedback data is essential to getting the most useful information from your feedback cycle. Without a tried and tested plan, it’s easy to miss a critical step or opportunity. That’s why we suggest following this simple yet effective feedback model.
5 practical steps to creating a successful feedback cycle
- Capture the information.
There are many ways to collect feedback from your patients – each with its benefits and limitations. Since every organisation is different, you’ll need to select the collection technique that suits your needs and the type of data you’re seeking.
Here are some examples of patient feedback collection methods:
- Patient experience surveys
This may consist of general information about patient needs, wants and pain points. SMS or automated kiosks are great platforms for this style of survey.
NEXA Voice is an excellent solution here as it can enable real-time reporting that can be accessed at any time. To learn more, visit our NEXA Voice information page.
- Tailored surveys
This prompts responses about a specific topic, location, department, clinic and more, and is great for targeted information about the patient experience.
- Population surveys
These are used to collect information about patients from diverse geographic and demographic backgrounds which can uncover community-specific issues.
- Focus groups
This type of survey is effective for collecting qualitative information from sample groups within a closed setting.
- Data analysis.
Your data is only useful if it can be understood. So, make sure that insights are translated into actionable and measurable outputs that can be reviewed over time.
Recording key findings and comparing the results against feedback collected down the track will allow you to spot patterns, opportunities for improvement and gaps requiring further attention.
- Communicate the feedback.
You’ve taken the time to ask for patient input. So, now you can share the insights you’ve worked so hard to uncover!
This will promote transparency within your facility about the feedback process and can promote internal discussions that will lead to potential improvements in your decision-making strategy.
- Implement the change.
At this point, you can start planning and implementing the changes developed from the previous steps. Depending on the type of improvement for your healthcare facility, we recommend the following tips:
- Set goals and objectives that are achievable, measurable and have a deadline.
- Establish manageable steps to achieving them.
- Prioritise your actions.
- Involve relevant stakeholders.
- Establish a reporting channel from start to finish.
- Measure your success.
After you’ve established targets, now is the time to review your results and monitor whether you are achieving what you set out to do.
This stage doesn’t have to feel like a criticism or a “once-off”. It’s more of an ongoing checkpoint to ensure things are progressing well. This way, your team can see if KPIs are being met to create a better patient experience and if further tweaks are needed.
Capturing and acting on feedback benefits everyone
Collecting, understanding and acting upon feedback can lead to long-term benefits for your patients, staff members and the entire health facility as improvements streamline the process, reduce wait times and improve efficiencies.
Engaging patients in the process and sharing the outcomes of the changes you devise is an effective way of showing them they are valued. Likewise, staff members who see your commitment to the continuous improvement and development of your facility can make them feel good about where they work and be more willing to contribute to its success.
Do you need help to improve the patient experience?
If your healthcare facility is looking to improve the overall patient experience but you’re still unsure of where to start, NEXA is here to support you.
NEXA is an Australian company that delivers innovative solutions that streamline the patient journey. We offer tailored software that empowers our clients to improve their service by taking advantage of digital technology. With NEXA’s solutions, you can support and enable your team, deliver excellent service and thrive in today’s evolving landscape..
Talk to us today to find out how we can help streamline your patient journey and improve your patient flow.